5 Postpartum Pelvic Floor Exercises Every Mom Should Try
Pregnancy and childbirth challenge the pelvic floor muscles through stretching, pressure, and potential trauma. These gentle exercises support postpartum recovery by rebuilding strength, coordination, and function.
Published January 13, 2026

Leaking when you sneeze or feeling like your body isn’t quite holding together yet? These worries are common after birth, but they’re often pushed aside while you focus on your newborn. Your pelvic floor has been under months of pressure and significant strain from delivery or surgery, so it’s normal for things to feel off at first.
This post shows how targeted, evidence-based exercises can help restore strength, improve bladder control, and support recovery at every stage. You’ll learn which movements are safe to start early, how to progress as you heal, and how to rebuild confidence in your body again.
What You Need to Know about the Pelvic Floor
The pelvic floor is a group of muscles that support your bladder, uterus, and bowel [1]. Pregnancy and birth, whether vaginal or via C-section, place heavy strain on these muscles, which is why recovery is needed afterward.
When You Can Begin Exercising
Gentle breathing and light pelvic floor activation can usually begin right after birth. More intense core work, especially after a C-section, will require you to wait until around six weeks. Always follow medical guidance — checking with your doctor to get their recommendation for your specific case is always a good idea.
Remember to never do Kegel exercises while urinating. This can interfere with normal bladder function and cause problems over time.
When to See a Pelvic Floor Physical Therapist
Pelvic floor physical therapists are the gold standard for postpartum recovery. Everyone benefits from professional assessment, but it's particularly important after:
- Perineal tearing or episiotomy (tear or small surgical cut in the area between the vagina and anus during childbirth)
- Cesarean delivery
- Pain during movement, exercise, or intercourse
These specialists identify whether muscles need strengthening or relaxation, correct technique errors, and create personalized progression plans.
5 Postpartum Pelvic Floor Exercises to Support Recovery
1. Diaphragmatic Breathing
You can begin diaphragmatic breathing immediately after delivery—even in the recovery room. The diaphragm (the large dome-shaped muscle beneath the lungs) sits at the top of the core, while the pelvic floor forms the bottom.
During inhalation, the diaphragm flattens downward to create space for the lungs. This gentle pressure travels through the abdomen to the pelvic floor, allowing those muscles to stretch and lengthen slightly. On exhalation, the diaphragm returns upward, pressure decreases, and the pelvic floor returns to resting position.
This gentle rhythmic movement increases blood flow to healing tissues and mobilizes the pelvic floor without any force or strain, making it ideal when tissue trauma prevents more active exercise.
- Lie on your back or sit comfortably
- Place one hand on the chest and one on the belly
- Inhale slowly through the nose for 4 seconds, focusing on expanding the ribcage outward like an umbrella opening—not just pushing the belly up
- The chest and shoulders should stay relatively quiet and relaxed
- Exhale slowly through the mouth for 4 seconds, allowing the ribs to return inward.
Try to avoid breathing too shallowly into just the upper chest, tensing shoulders, or forcing the belly to expand rather than allowing natural rib expansion.
Practice 10 breaths twice daily, or whenever needed for relaxation and recovery. You can progress by gradually lengthening both inhale and exhale to 6-8 seconds each and more thereafter. Stop if dizziness occurs and return to normal breathing.
Beyond pelvic floor mobilization, diaphragmatic breathing activates gentle abdominal engagement, encourages intestinal movement (helpful for postpartum constipation), and reduces stress through parasympathetic nervous system (the body's relaxation system) activation [2].
2. Kegel Exercises (Pelvic Floor Muscle Training)
After months of pressure and the stretching or trauma of delivery, pelvic floor muscles need gentle reactivation to restore their ability to contract, support pelvic organs, and maintain continence.
Kegels, especially when done correctly using biofeedback therapy training, teach these muscles to squeeze and lift on command, rebuilding the strength and coordination lost during pregnancy and birth [3].
First, identify the correct muscles:
Squeeze your muscles as if you're trying to stop urine flow midstream or prevent passing gas. Both sensations are correct—the pelvic floor spans front to back, controlling both openings.
To perform:
Inhale and let everything relax completely
On the exhale, gently squeeze and lift those muscles upward toward the head, as if pulling them up inside
Hold briefly, then fully relax on the inhale
If the abdominal muscles, inner thighs, or buttocks are visibly tensing, stop and reset. Those muscles should stay relatively quiet. The pelvic floor works independently from these larger muscle groups
Early Postpartum (First 2-3 weeks): Aim for gentle 1-second holds, 5 repetitions, 5 times daily
As Strength Improves (Weeks 3-6): Progress to 10 repetitions per set, gradually increasing hold time up to 10 seconds
Try not to exceed 30-50 repetitions total per day; more is not better. Overworking pelvic floor muscles can cause soreness, fatigue, and paradoxically worsen symptoms.
Do not perform Kegels if on pelvic rest (doctor's orders to avoid vaginal activity) or if a healthcare provider specifically advises against them.
Some women experience pelvic floor hypertonicity (overly tight muscles that need pelvic floor relaxation, not strengthening).
If you need pelvic floor relaxation down training, you may experience pain during Kegels, painful intercourse, or difficulty fully emptying the bladder.
Strengthening pelvic floor muscles improves more than just bladder control. Many women notice improved sensation during intercourse, better support of pelvic organs, and increased confidence during physical activity [4].
Strength improvements typically become noticeable after 4-6 weeks of consistent practice, though some symptom relief may appear earlier.
3. Transverse Abdominis Activation
The transverse abdominis (TA) is the deepest layer of abdominal muscles, wrapping around the torso from front to back like a corset [6]. After months of stretching to accommodate pregnancy, and particularly after a cesarean delivery that cuts directly through abdominal tissue, the TA often struggles to contract effectively.
Rebuilding TA strength provides support for the spine and pelvic floor during daily activities like lifting, carrying, and bending. Studies show TA activation reduces lumbar instability, which is particularly relevant given the postpartum combination of core weakness and the physical demands of infant care [7].
This exercise can be practiced in various positions, including lying on your back, sitting, standing, or even on your hands and knees. Choose whichever position makes the muscle engagement most noticeable.
Inhale and relax completely
On the exhale, imagine zipping up a pair of jeans that are slightly too tight, starting from the pubic bone and pulling upward to the sternum (breastbone)
This should feel like someone gently tightening a corset around the midsection—not sucking in the stomach or pushing the belly outward
The movement is subtle. The abdominal wall should draw inward and slightly upward, but not dramatically
Shoulders must stay relaxed, and breathing continues normally (don't hold your breath)
Start with 10 repetitions, 2-3 times daily, and improve from there. Once the activation feels natural and controlled, begin incorporating it into functional movements like engaging the TA before lifting the baby, pushing a stroller, or getting up from the floor.
Later progression includes adding TA activation to other exercises like planks, squats, or deadlifts for increased core stability.
Stronger core muscles improve posture, reduce lower back pain, and make prolonged sitting or standing more comfortable—all common postpartum concerns [8]. Many women notice better posture and easier movement after 3-4 weeks of consistent practice as core support systems rebuild.
Keep in mind that after cesarean delivery, you should check with your OB-GYN before starting TA exercises to ensure the incision has healed sufficiently.
4. Glute Bridges
Bridges rebuild strength in the glutes (buttock muscles), hamstrings (back of thighs), and core while improving hip and pelvic stability.
When these muscles provide better support and stability, the pelvic floor doesn't have to work as hard to compensate—allowing it to focus on its primary functions of continence and organ support [9].
Bridges are also essential for functional movements like rolling in bed, getting up from seated positions, and transitioning from lying to standing—all movements performed dozens of times daily with a newborn.
Lie on your back on a firm surface (floor or firm mattress)
Bend both knees and place feet flat on the surface at a comfortable distance from the buttocks—typically hip-width apart
Exhale while lifting the hips and buttocks upward until the front of the hips and thighs form a straight line
Do not overextend into the lower back by lifting too high
Inhale while lowering back down in a controlled motion
Keep both hip bones level throughout the movement—don't allow one side to hike up higher than the other
Start with 5-10 repetitions for 1-3 sets, twice daily. Some progression options, as your strength improves, can include:
- Increase repetitions to 15-20 per set
- Stagger foot position (one foot slightly ahead of the other)
- Add weight across the hips
- Progress to single-leg bridges
Improved glute and hip strength makes moving in bed easier, reduces struggle when standing from seated positions, and supports longer periods of standing with better posture.
Like most strength exercises, noticeable improvements typically appear after 4-6 weeks of consistent practice, though functional benefits build progressively.
5. Side-Lying Hip Abduction
Hip abductor muscles (located on the outer hip) provide critical pelvic stability, which becomes especially important after pregnancy hormones like relaxin have loosened the ligaments and muscles surrounding the pelvis [10].
Strong hip abductors make daily activities easier, like climbing stairs, standing from chairs, balancing, and squatting down to pick things up. They're also essential for walking and running mechanics.
When hip abductors provide good stability, the pelvic floor doesn't need to overwork to compensate.
Lie on one side of the body. The head can rest on the bottom arm for comfort
Bend the bottom leg slightly for stability, but keep the top leg straight with the ankle in line with the shoulder
Exhale while lifting the top leg upward until it's level with the hip or slightly higher
Inhale while slowly lowering back down with control
Repeat on the same side, then switch
Important Cue: Do not lift so high that the waist bends or the torso rolls backward. This is a hip exercise—the waist should stay stable and straight.
Perform 2 sets of 10 repetitions on each side, twice daily.
Some progression options for you include:
- Straighten the bottom leg for an increased stability challenge
- Add ankle weights or resistance bands
- Increase repetitions to 15-20 per set
Although it's not a direct pelvic floor exercise like Kegels, hip abductors provide essential pelvic stability during single-leg activities like walking. This becomes particularly important after relaxin has decreased joint stability throughout the pelvis.
Moving Forward With Your Recovery
Postpartum pelvic floor issues like leaking, weakness, and pressure are common, but they don’t fix themselves overnight. These muscles have been through months of strain and need the right support to recover safely and fully.
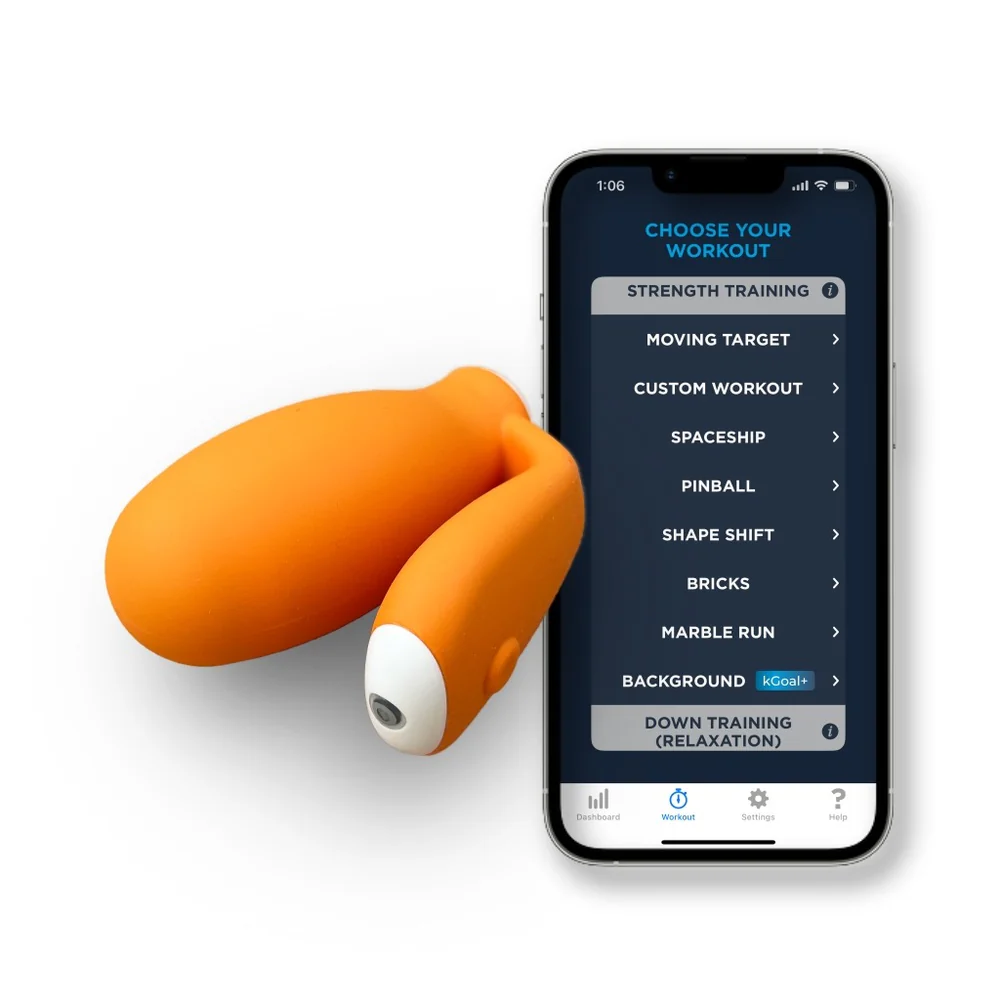
The solution is starting gently and staying consistent. Simple exercises, especially Kegels that are done correctly, help rebuild strength over time. Tools like those from kGoal guide proper technique from the start, making it easier to stay on track, see progress, and support real recovery.
References
1. Professional, C. C. M. (2025, December 19). Pelvic floor muscles. Cleveland Clinic. https://my.clevelandclinic.org/health/body/22729-pelvic-floor-muscles
2. Grogan, J. (2025, November 17). Diaphragmatic breathing for pelvic floor health. Alliance Physical Therapy Partners. https://carolinastrongpt.com/diaphragmatic-breathing-pelvic-floor/
3. Huang, Y., & Chang, K. (2023, May 1). Kegel exercises. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK555898/
4. Stamos, D., Sapouna, V., Astraka, K. M., Thanopoulou, S., Giannakis, I., Pantou, A., Baltogiannis, D., Paschopoulos, M., Sofikitis, N., & Zachariou, A. (2025). Female Sexual Function and Pelvic floor Muscle Training: A Narrative review. Cureus, 17(6), e85751. https://doi.org/10.7759/cureus.85751
5. Kandadai, P., O’Dell, K., & Saini, J. (2014). Correct performance of pelvic muscle exercises in women reporting prior knowledge. Female Pelvic Medicine & Reconstructive Surgery, 21(3), 135–140. https://doi.org/10.1097/spv.0000000000000145
6. Transversus abdominis. (n.d.). Physiopedia. https://www.physio-pedia.com/Transversus_Abdominis
7. Ali, M. G., Yousef, A. M., Sarhan, M. a. M., Alwhaibi, R. M., Zakaria, H. M., Mohammed, A. A., Ragab, W. M., Mamoon, R. S., & Auais, M. (2025). Testing the Association Between Low Back Pain Intensity and Core Muscle Strength in Postpartum Women with Different Delivery Modes: An Analytical Cross-Sectional Study. Journal of Clinical Medicine, 14(18), 6505. https://doi.org/10.3390/jcm14186505
8. Vesting, S., Gutke, A., & De Baets, L. (2025). Educating women to prevent and treat low back and pelvic girdle pain during and after pregnancy: a systematized narrative review. Annals of Medicine, 57(1), 2476046. https://doi.org/10.1080/07853890.2025.2476046
9. Lehecka, B., Edwards, M., Haverkamp, R., Martin, L., Porter, K., Thach, K., Sack, R. J., & Hakansson, N. A. (2017, August 1). BUILDING a BETTER GLUTEAL BRIDGE: ELECTROMYOGRAPHIC ANALYSIS OF HIP MUSCLE ACTIVITY DURING MODIFIED SINGLE-LEG BRIDGES. https://pmc.ncbi.nlm.nih.gov/articles/PMC5534144/
10. Hip abductors. (n.d.). Physiopedia. https://www.physio-pedia.com/Hip_Abductors
FAQs
How does pregnancy and childbirth affect the pelvic floor structurally?
Pregnancy increases weight and pressure on pelvic floor muscles for months while hormones like relaxin loosen the ligaments that stabilize the pelvis. Vaginal delivery involves major muscle stretching and possible tearing or episiotomy trauma. Cesarean section cuts through multiple abdominal muscle layers, disrupting core support. All delivery methods challenge the pelvic floor significantly, requiring dedicated recovery regardless of how the baby arrived.
Why shouldn't active exercise start immediately after delivery?
Actually, gentle exercises like diaphragmatic breathing and light Kegels can often begin immediately after delivery unless specifically contraindicated by a healthcare provider. The caution applies to high-impact or strenuous exercise. Tissue needs time to heal from tears, incisions, or stretching trauma. Jumping into intense activity too soon risks delayed healing, worsening symptoms, or causing new injuries like prolapse.
What warning signs mean someone needs professional pelvic floor assessment?
Seek pelvic floor physical therapy evaluation for: urinary or fecal incontinence, pelvic pain during movement or intercourse, feeling of heaviness or pressure suggesting prolapse, inability to identify or activate pelvic floor muscles, pain during Kegel exercises, significant tearing or episiotomy, or cesarean delivery. While assessment benefits all postpartum mothers, these symptoms particularly indicate the need for professional guidance.
Can Kegels be performed while urinating to check if the right muscles are working?
No—never practice Kegels while actually urinating. While the "stop urine midstream" instruction helps identify which muscles to engage, regularly performing Kegels during urination can confuse bladder signals and train the pelvic floor to contract when it should fully relax for emptying. This can lead to incomplete bladder emptying and increased infection risk.
How soon after cesarean delivery can abdominal exercises begin?
Gentle diaphragmatic breathing can typically begin immediately. Transverse abdominis activation and more active abdominal work should wait until the OB-GYN provides clearance, usually around six weeks, but sometimes longer, depending on surgical complexity or healing progress. Always follow specific provider guidance and stop immediately if incision pain occurs.
Why do some women experience pelvic pain during Kegel exercises?
Pain during Kegels often indicates pelvic floor hypertonicity—muscles that are overly tight rather than weak. These muscles need relaxation and "down training" rather than strengthening. Attempting to strengthen already tight muscles can worsen pain and dysfunction. Pelvic floor physical therapists can assess muscle tone and prescribe appropriate treatment, which may include manual therapy, stretching, or relaxation exercises instead of Kegels.